Understanding Insulin Resistance
Insulin resistance is a condition characterized by decreased sensitivity to insulin, resulting in the hormone's reduced effectiveness in regulating blood glucose levels. While the precise reasons for insulin resistance remain elusive, advancements in scientific research have shed light on its development and potential interventions.
In this blog post, we will delve into the science behind insulin resistance, explore its causes, and provide tangible examples of what can be done to mitigate its effects on health.
What is Insulin?
To comprehend insulin resistance better, it is essential to first understand what insulin is and its vital role in the body's glucose regulation system. Think of insulin as a key that unlocks the doors of your body's cells to allow glucose, the primary source of energy, to enter. This analogy will help illustrate the significance of insulin and how its dysfunction can lead to insulin resistance.
Imagine your body's cells as individual rooms in a large building, and glucose as the fuel required to power all the activities happening inside each room. Now, picture insulin as a key that fits perfectly into the locks on these room doors, allowing glucose to enter and provide energy to the cells.
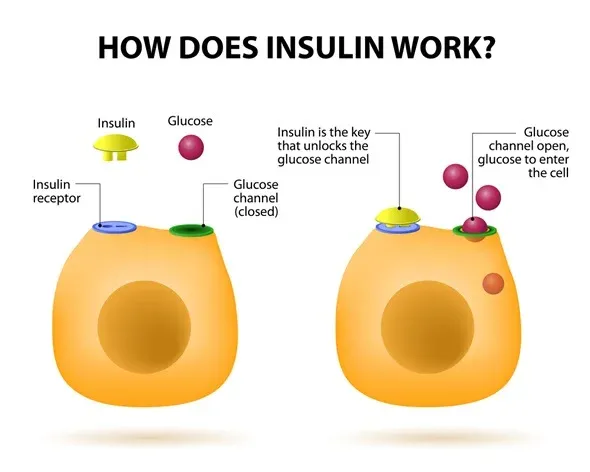
When everything functions optimally, insulin is produced by the pancreas in response to elevated blood glucose levels after a meal. It acts as the key, opening the doors of the cells and enabling glucose to enter. The cells then utilize this glucose as fuel for various processes, such as muscle contraction or brain function.
However, in the case of insulin resistance, the lock mechanism on the cell doors becomes less responsive to the insulin key. It's as if the locks have become rusty or resistant to turning. As a result, the glucose struggles to enter the cells efficiently, leading to elevated levels of glucose in the bloodstream.
To compensate for this resistance, the body produces more insulin, akin to creating additional copies of the key to force open the resistant locks. Initially, this surge of insulin can overcome the resistance and allow glucose to enter the cells. However, over time, the resistance may worsen, making it increasingly challenging for insulin to do its job effectively. This is similar to needing more and more copies of the key to unlock the stubborn doors.
Eventually, the pancreas, which is responsible for producing insulin, may struggle to keep up with the demand for higher insulin levels. The lock mechanism becomes more resistant, and the pancreas may even tire out from the constant production of insulin. This can lead to a decrease in insulin production, making it even harder for glucose to enter the cells. The result is elevated blood glucose levels, a hallmark of prediabetes or type 2 diabetes.
By understanding the crucial role of insulin and the impact of insulin resistance, we can appreciate the importance of addressing this condition and implementing strategies to improve insulin sensitivity.
Causes of Insulin Resistance:
- Genetic Factors: Certain genes can predispose individuals to develop insulin resistance, influencing their susceptibility to the condition.
- Age: Aging is linked to an increased likelihood of insulin resistance, highlighting the importance of proactive health measures as we grow older.
- Lifestyle Factors: Sedentary behavior, obesity, and being overweight contribute to insulin resistance. Excess fat tissue may trigger inflammation, stress, or cellular changes that impair insulin sensitivity. Additionally, there may be unidentified factors produced by fat tissue that induce insulin resistance.
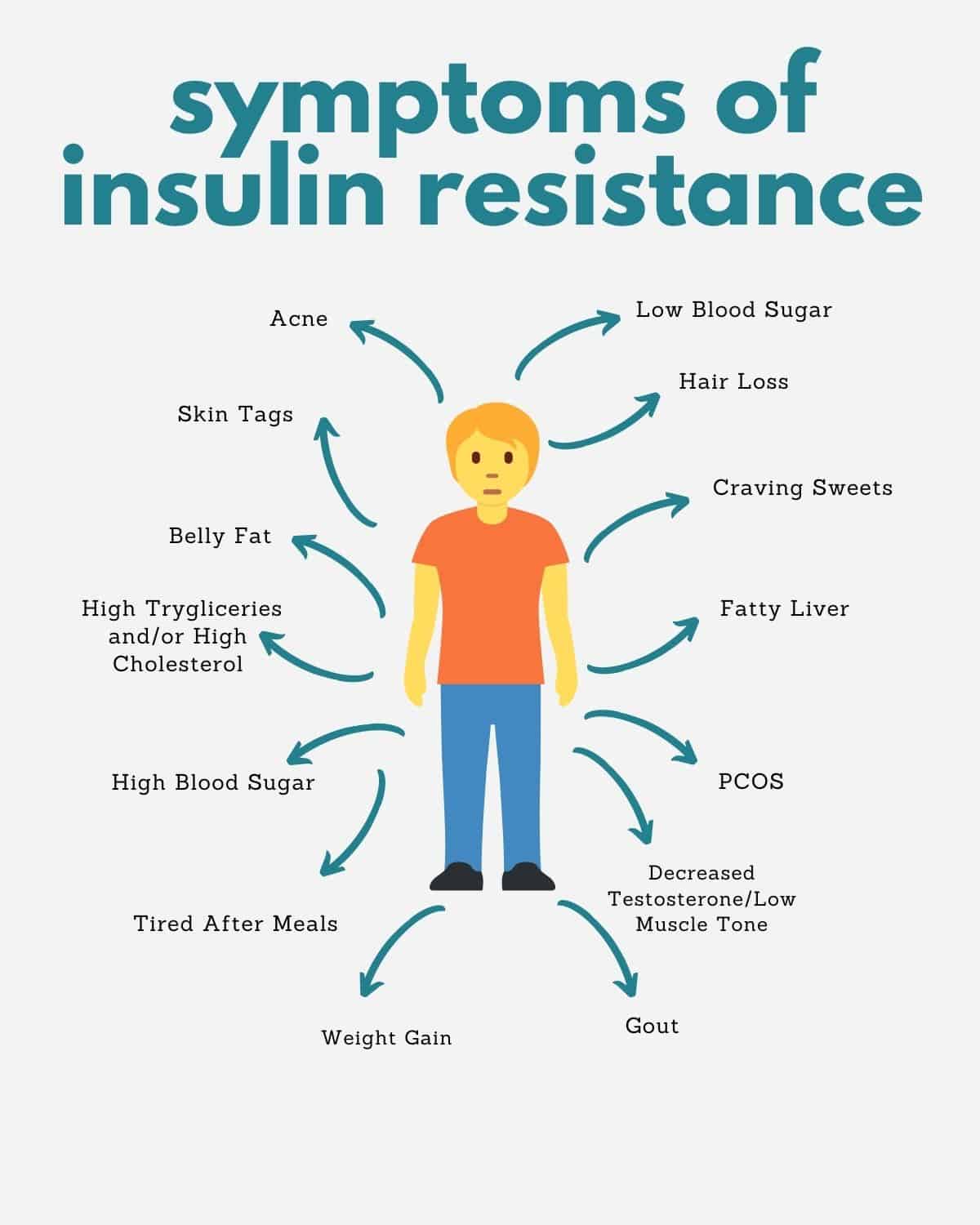
Impact on Health:
Insulin resistance exists on a spectrum, affecting both type 1 and type 2 diabetes differently:
- Type 2 Diabetes: The severity of insulin resistance directly correlates with the challenge of managing diabetes. Higher insulin doses may be required to achieve target blood glucose levels in individuals with significant insulin resistance.
- Type 1 Diabetes:While insulin resistance is not a cause of type 1 diabetes, those with type 1 who are insulin resistant may need higher insulin doses for effective blood glucose control. Insulin resistance may also contribute to cardiovascular disease and other complications in type 1 diabetes.
Strategies for Managing Insulin Resistance:
- Physical Activity: Engaging in regular exercise is crucial for combating insulin resistance. Exercise enhances insulin sensitivity, builds muscle mass that aids glucose absorption, and offers an alternative pathway for glucose uptake without insulin mediation. These effects improve blood glucose control and overall insulin responsiveness.
- Weight Loss: Shedding excess weight has a positive impact on insulin resistance. Although no single diet is universally proven to be most effective, evidence suggests that low-fat, high-carbohydrate diets may exacerbate insulin resistance.
- Medications: While no specific medications are approved to treat insulin resistance, certain diabetes medications like metformin and thiazolidinediones (TZDs) can reduce insulin resistance and lower blood glucose levels.
Insulin resistance poses challenges for individuals with diabetes, but proactive measures can enhance insulin sensitivity and improve overall health:
- Embrace an active lifestyle to boost insulin sensitivity and glucose control.
- Strive for a healthy weight through balanced nutrition and weight-loss strategies.
- Consider diabetes medications that can help combat insulin resistance.
Remember, you are not alone in the fight against insulin resistance. By implementing these strategies and working closely with healthcare professionals, you can regain control over your blood glucose levels and improve your overall well-being.