The Role of Fats in Insulin Resistance

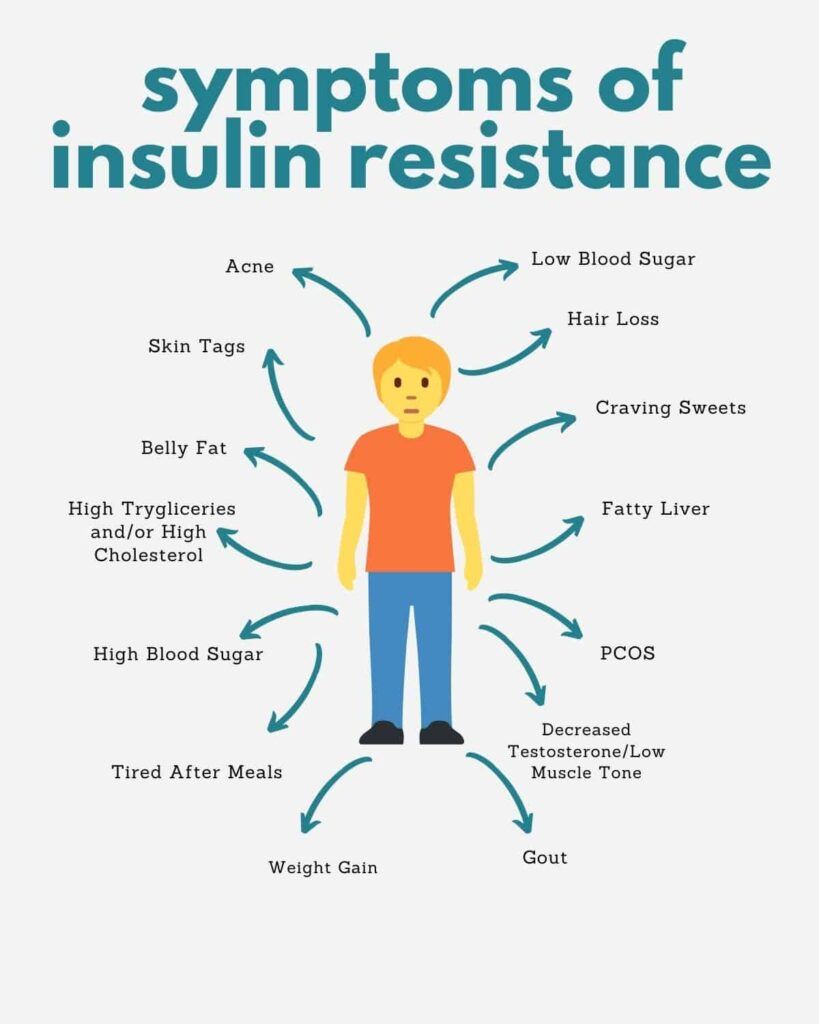
Insulin resistance is a complex condition where the body's cells don't respond effectively to insulin, a hormone that regulates blood sugar. One of the primary causes of insulin resistance is inflammation, which can be influenced by the types of fats we consume. This article delves into the intricate relationship between different fatty acids, inflammation, and insulin resistance, and how they impact various organs in our body.
What is Insulin Resistance?
Insulin resistance is a condition where the body's cells become less responsive to the hormone insulin. Imagine insulin as a key and the cells as locks. In a healthy scenario, insulin (the key) fits perfectly into the cells (the locks) to let glucose (sugar) in.
However, with insulin resistance, it's as if the locks become rusty, making it harder for the key to work effectively. As a result, more and more insulin is needed to achieve the same effect, leading to higher levels of both insulin and glucose in the blood.
The Role of Inflammation:
Inflammation is the body's natural response to injury or infection. However, chronic inflammation, especially when it's not due to an apparent injury or infection, can be problematic. One of the main culprits behind this type of inflammation is our diet, particularly certain types of fats.
- Omega-6 Fats: Found in many vegetable oils and processed foods, omega-6 fats, when consumed in excess, can promote inflammation. While they are essential in small amounts, the modern diet often contains far more omega-6 fats than our bodies need, tipping the balance towards inflammation.
- Saturated Fats: Commonly found in animal products like meat and dairy, as well as some tropical oils, saturated fats can activate certain pathways in the body that lead to inflammation.
On the flip side:
- Omega-3 Fats: These are the "good guys" when it comes to inflammation. Found in fatty fish, walnuts, and flaxseeds, omega-3 fats can counteract inflammation, helping to restore balance in the body.

How Different Organs Are Affected:
Different organs in our body can be impacted by these dietary fats and the resulting inflammation:
- Liver: The liver is a powerhouse organ responsible for processing and storing nutrients. When it's bombarded with unhealthy fats, it can become inflamed and start to store excess fat, leading to conditions like non-alcoholic fatty liver disease (NAFLD). Over time, this can make the liver less responsive to insulin.
- Muscles: Our muscles use glucose as a primary source of energy. However, when they become inflamed due to an excess of unhealthy fats, they can become resistant to insulin, meaning they struggle to take in glucose from the blood.
- Brain (Hypothalamus): The hypothalamus is a small but vital part of the brain that regulates hunger and energy expenditure. Inflammation here, often triggered by saturated fats, can disrupt its normal functioning. This can lead to increased feelings of hunger and a decreased sense of fullness after eating, contributing to overeating and weight gain.
- Adipose Tissue (Fat Cells): While fat cells are designed to store excess energy, they can become inflamed and resistant to insulin when they expand too much. This can lead to more fat being stored in other organs like the liver.
Applying This Knowledge to Everyday Life:
Mind Your Fats: A Closer Look at Dietary Fats
- Why it Matters: The types of fats we consume can either promote or reduce inflammation, which plays a pivotal role in insulin resistance. Making the right choices can help manage or even prevent this condition.
- Guidelines:
- Increase Omega-3 Intake: Foods rich in omega-3 fatty acids, such as fatty fish (salmon, mackerel, sardines), walnuts, chia seeds, and flaxseeds, can help reduce inflammation.
- Limit Saturated Fats: Reduce (not eliminate) consumption of red meats, full-fat dairy products, and tropical oils like coconut and palm oil.
- Watch Out for Omega-6: While omega-6 fats are essential, they're often overconsumed in modern diets. Limit intake of processed foods, fried foods, and certain vegetable oils like corn and soybean oil.
Stay Active: The Power of Movement
- Why it Matters: Physical activity helps muscles use glucose more efficiently, reducing the need for excessive insulin. This can help combat insulin resistance and its associated risks.
- Guidelines:
- Aim for Consistency: Engage in at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity every week.
- Incorporate Strength Training: Include muscle-strengthening activities on 2 or more days a week.
- Stay Flexible: Activities like yoga and stretching can improve flexibility and reduce stress, another factor that can contribute to insulin resistance.
Monitor Your Weight: The Link Between Weight and Insulin Sensitivity
- Why it Matters: Excess weight, especially around the abdomen, is a key risk factor for insulin resistance. Maintaining a healthy weight can significantly reduce this risk.
- Guidelines:
- Set Realistic Goals: Aim for a gradual weight loss of 200-400g per week. Rapid weight loss can be hard to maintain and may not be healthy.
- Balanced Diet: Focus on a diet rich in whole foods, including vegetables, fruits, lean proteins, and whole grains.
- Stay Hydrated: Drink plenty of water throughout the day, and limit sugary drinks and alcohol.
Understanding the role of dietary fats in insulin resistance is crucial for making informed dietary choices.
By being aware of how different fats impact our body and its organs, we can make choices that promote health and reduce the risk of conditions like diabetes. Remember, it's not just about the quantity of fats, but the quality!